Key points
Digestive diseases (excluding viral hepatitis and digestive cancers) represent a group of common conditions, especially among the elderly. In France, over 65 years old, 29% of the population report being affected by these diseases, which account for more than 10% of consultations in general practice. Digestive diseases are also the main diagnosis for over 10% of hospital stays in acute care services, nearly 1.8 million stays annually.
The Pays de la Loire region shows, with a comparable age structure, an 18% lower frequency of hospitalizations for these conditions compared to the national average. This lower hospitalization rate is observed for most digestive-related hospital admission reasons, including chronic liver diseases linked to excessive alcohol consumption, which was not previously the case. Although this hypothesis requires further confirmation, this trend likely reflects changes in healthcare management practices. Indeed, the frequency of admissions for long-term conditions (LTC) due to alcoholic liver disease remains significantly higher in Pays de la Loire than in France (+29%), and deaths related to these diseases are also more frequent in the region (+15%).
Regional mortality linked to digestive diseases has nevertheless clearly decreased in recent years. For example, Pays de la Loire, which had a male excess mortality due to digestive diseases in the 2000s, reached the national mortality level in 2009-2011.
Furthermore, the epidemiology of chronic inflammatory bowel diseases (IBD) is concerning. The regional frequency of LTC admissions for IBD has sharply increased in recent years (+6% per year on average between 2005 and 2012), following the same trend nationally. However, the regional frequency of these admissions remains 12% lower than the French average.
Situation in France
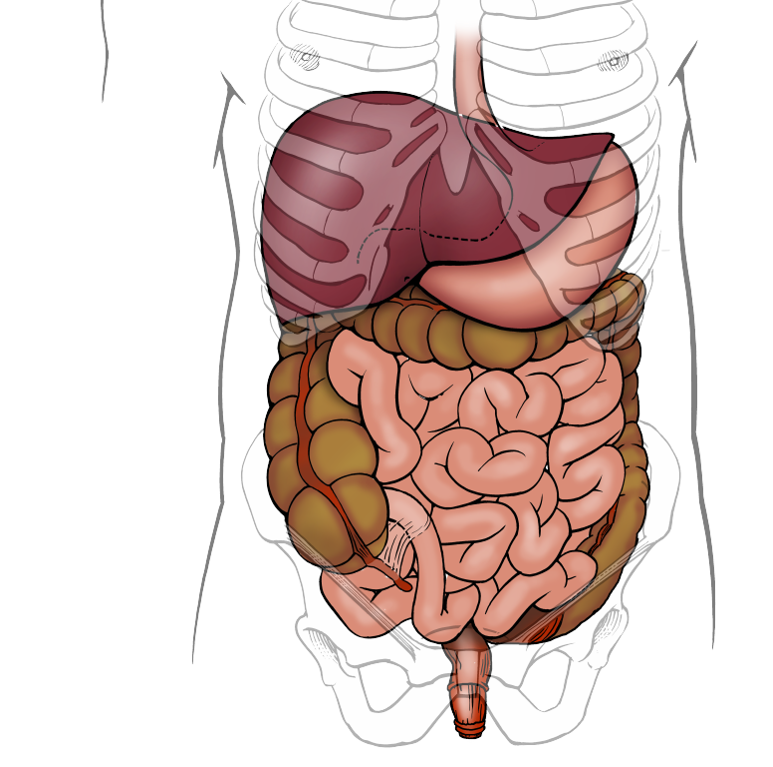
Digestive diseases comprise a variety of acute and chronic conditions with diverse natural histories, risk factors, and prognoses. They can affect the digestive tract (from the oral cavity to the rectum), the peritoneum, as well as the liver, biliary tract, and pancreas. Some of these conditions are both severe and relatively common, such as liver diseases and chronic inflammatory bowel diseases. Others are less severe but can significantly impair the quality of life of affected individuals (gastroesophageal reflux, functional intestinal disorders…) [1].
The pathologies described here correspond to those classified under the “Digestive Diseases” chapter in the International Classification of Diseases (ICD-10), excluding diseases of the teeth and periodontal tissue. Digestive cancers and diseases of endocrine or infectious origin (notably viral hepatitis), which represent a significant part of gastroenterologists’ work, are not included in this study.
Diseases that heavily engage the healthcare system
Digestive diseases are common: 16% of the general population in metropolitan France reported having them in 2010. This percentage increases with age, reaching 29% beyond 65 years [2].
In outpatient care, digestive diseases accounted for 3% of visits by people under 25 in 2011-2012. This proportion rises markedly with age, reaching 7-8% among adults aged 25 to 64 and over 10% among those aged 65 and above [2].
In healthcare facilities, digestive diseases were the primary diagnosis in 11% of stays in medicine-surgery-obstetrics (MCO) departments in metropolitan France in 2011 (nearly 1.8 million stays) [3]. The most frequent reasons for hospitalization are abdominal hernias (14%) and intestinal diverticulosis (10%). These conditions often undergo surgical or ambulatory medical treatment, partly explaining the high proportion of hospital stays under 24 hours for digestive diseases (49% in 2011). Short stays can also be linked to digestive endoscopies (diagnostic or therapeutic), with over 2 million performed annually in France [4].
Among stays over 24 hours, aside from abdominal hernias (17%), the most frequent causes for hospitalization are gallstones (15%), appendicitis (9%), and intestinal obstructions without hernia (7%) [3].
Two groups of chronic digestive diseases, requiring prolonged care, are recognized as long-term conditions (LTC) by health insurance: inflammatory bowel diseases (IBD), including ulcerative colitis and Crohn’s disease (LTC No. 24), and active chronic liver diseases and cirrhosis (which can be caused by excessive alcohol consumption, viruses, or biliary/metabolic damage; LTC No. 6).
IBD accounted for LTC admissions of nearly 13,600 people annually on average between 2011 and 2012 in metropolitan France [5]. At the end of 2012, nearly 142,600 people were registered as LTC patients for these diseases, 55% of whom had Crohn’s disease [6].
Active chronic liver diseases (excluding viral hepatitis) and cirrhosis were slightly less frequent LTC admission causes than IBD. Nearly 11,800 people were admitted to LTC annually on average between 2011 and 2012 [5]. By the end of 2012, the total number of LTC patients for active chronic liver diseases was estimated at nearly 91,800, 45% of whom had alcoholic liver diseases and 44% had fibrosis or cirrhosis of non-alcoholic origin [6].
Digestive diseases caused nearly 23,100 deaths annually on average in metropolitan France during 2009-2011, representing 4% of all deaths [7].
The severity of liver diseases explains their large share of digestive mortality: 31% of digestive deaths are related to chronic liver disease (41% in men, 19% in women), mostly of alcoholic origin.
The majority of deaths caused by chronic liver disease occur before age 65 (60%), compared to only 16% for all other digestive-related causes.
Marked regional disparities
Within France, the frequency of hospitalizations for digestive diseases varies significantly by region. In mainland France, Île-de-France (+6% compared to the national average), northern regions (Picardie +6%, Nord-Pas-de-Calais +13%), and especially southeastern regions (Languedoc-Roussillon +11%, Provence-Alpes-Côte d’Azur +25%, Corsica +48%) showed the highest age-adjusted hospitalization rates in 2011. Western regions (Pays de la Loire -18%, Brittany -16%, Lower Normandy -15%) showed the lowest rates.
These regional differences have multiple causes. Besides the epidemiology of each digestive disease, differences in healthcare practices and, to a lesser extent, hospital coding practices, partially explain these disparities.
There are also territorial disparities in LTC admissions. Overseas departments show the lowest age-adjusted LTC admission rates for IBD in 2011-2012. In mainland France, the highest rates are in northern and southeastern regions, while central regions have more favorable situations. A decreasing North-South gradient is classically described in the literature for IBD frequency [8], though precise reasons remain poorly documented. Regional differences in LTC admissions may also partly result from medico-administrative factors.
Differences in LTC admissions are even more marked for active chronic liver diseases. Northern and western regions, especially Nord-Pas-de-Calais, have the highest rates, whereas southern regions and Île-de-France have more favorable situations. These disparities partly align with regional alcohol consumption differences [9].
Comparative indices of LTC admissions for digestive diseases
France overall (2011-2012 average):
Adjusted for age structure, Île-de-France and southern regions show the lowest mortality rates from digestive diseases in metropolitan France. In contrast, northern regions, especially Nord-Pas-de-Calais, have significantly worse outcomes compared to the national average.
Increasing disease frequency but decreasing mortality
Between 1998 and 2011, the age-standardized hospitalization rate for digestive diseases increased by 0.3% per year on average for men and 0.6% for women [2].
LTC admissions for digestive diseases are also rising, mainly due to a sharp increase in LTC admissions for IBD (+4.9% per year for men and +4.7% for women between 2005 and 2012) [5]. These data align with national and international epidemiological studies showing increased IBD incidence in industrialized and developing countries [8].
The standardized LTC admission rate for active chronic liver diseases (excluding viral hepatitis) also rose, but less sharply: +1.6% per year for men and +0.8% for women.
In contrast, the standardized mortality rate from digestive diseases improved considerably, decreasing by 1.9% per year for men and 2.2% for women between 2000-2002 and 2009-2011 [7].
The decline in mortality from alcoholic liver disease and cirrhosis of unspecified origin was especially marked: -3.0% per year for men and -3.5% for women.
Evolution of standardized mortality rate from digestive diseases
Pays de la Loire, Metropolitan France (2000-2011)
Sources: Inserm CépiDc, RP (Insee)
3-year smoothed data – Unit: per 100,000
Standardized to European population
Is prevention of some digestive diseases possible?
Beyond improving survival in the most severe conditions, current health policies also aim to improve quality of life for people with common conditions such as functional digestive disorders, gastroesophageal reflux, or proctological diseases, and to develop ambulatory, non-invasive management of IBD [8].
Preventing digestive diseases, especially severe and disabling ones, is also important. IBD has multifactorial origins—both genetic and environmental—with poorly understood mechanisms. Several risk factors are under study, but to date, the only confirmed environmental risk factor for Crohn’s disease is smoking, which paradoxically appears protective for ulcerative colitis [8][10].
Main risk factors for non-viral chronic liver diseases and cirrhosis are overweight/obesity and prolonged excessive alcohol consumption. Hence, the occurrence and worsening of chronic liver diseases can partly be prevented by risk behavior reduction actions [11][12]. Chronic liver disease is insidious and